Page 36 - 2016-2021-ASU
P. 36
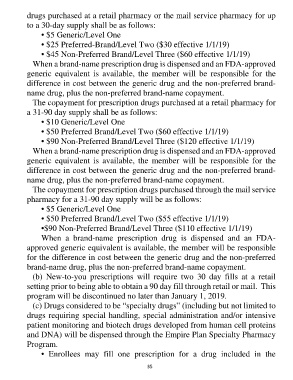
drugs purchased at a retail pharmacy or the mail service pharmacy for up
to a 30-day supply shall be as follows:
• $5 Generic/Level One
• $25 Preferred-Brand/Level Two ($30 effective 1/1/19)
• $45 Non-Preferred Brand/Level Three ($60 effective 1/1/19)
When a brand-name prescription drug is dispensed and an FDA-approved
generic equivalent is available, the member will be responsible for the
difference in cost between the generic drug and the non-preferred brand-
name drug, plus the non-preferred brand-name copayment.
The copayment for prescription drugs purchased at a retail pharmacy for
a 31-90 day supply shall be as follows:
• $10 Generic/Level One
• $50 Preferred Brand/Level Two ($60 effective 1/1/19)
• $90 Non-Preferred Brand/Level Three ($120 effective 1/1/19)
When a brand-name prescription drug is dispensed and an FDA-approved
generic equivalent is available, the member will be responsible for the
difference in cost between the generic drug and the non-preferred brand-
name drug, plus the non-preferred brand-name copayment.
The copayment for prescription drugs purchased through the mail service
pharmacy for a 31-90 day supply will be as follows:
• $5 Generic/Level One
• $50 Preferred Brand/Level Two ($55 effective 1/1/19)
•$90 Non-Preferred Brand/Level Three ($110 effective 1/1/19)
When a brand-name prescription drug is dispensed and an FDA-
approved generic equivalent is available, the member will be responsible
for the difference in cost between the generic drug and the non-preferred
brand-name drug, plus the non-preferred brand-name copayment.
(b) New-to-you prescriptions will require two 30 day fills at a retail
setting prior to being able to obtain a 90 day fill through retail or mail. This
program will be discontinued no later than January 1, 2019.
(c) Drugs considered to be “specialty drugs” (including but not limited to
drugs requiring special handling, special administration and/or intensive
patient monitoring and biotech drugs developed from human cell proteins
and DNA) will be dispensed through the Empire Plan Specialty Pharmacy
Program.
• Enrollees may fill one prescription for a drug included in the
35